The ability to isolate and assay circulating cell-free DNA from plasma holds promise for improved diagnostics and treatment in the clinic. The use of blood-based non-invasive prenatal testing (NIPT) has been well described. Such testing is based on circulating cell-free fetal DNA in blood of a pregnant woman for diagnosis and screening of chromosomal anueploidy (e.g. Trisomy 21, Down Syndrome), sex-linked diseases, and genetic diseases that are known to result from a specific mutation in a single gene (1). Additionally, most cancers carry somatic mutations that are unique to the tumors, and dying tumor cells release small pieces of their DNA into the blood stream (2). This circulating cell-free tumor DNA can be used as a biomarker to “follow” cancer progression or regression during treatment, and diagnostic methods also are being developed to detect even early stage cancers from circulating tumor DNA (3). Further, increases in circulating cell-free DNA have been well documented after intense exercise, trauma, sepsis and even associated with autoimmune diseases such as system lupus erythematosus (SLE; 1,4). In these latter examples increases in extracellular DNA are associated with evolutionarily conserved innate immune responses involving the production of neutrophil extracellular traps (NETs). Monitoring the circulating cell-free DNA of NETs has implications for treatment and diagnosis of autoimmune diseases, cardiovascular events and traumatic injuries (4–7).
How Neutrophils Weave a Defensive Web
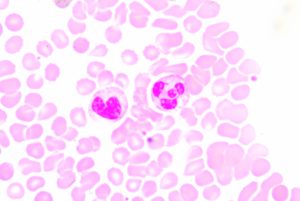
Neutrophils are the most abundant type of white blood cell and are part of the innate immune response, participating in non-specific immune responses to injury or pathogens. They are one of three types of granuolcytes, and can be recognized by their multi-lobed nucleus and the prominent granules that fill their cytoplasm. Generally they are first to the scene of injury or infection. Early in my scientific career, I was taught that neutrophils fought disease via phagocytosis and occasionally by firing a barrage of toxic enzymes and molecules at invaders. Mostly though they released cytokines that recruited the “important” cells of the specific immune system to the area.
For these reasons, I never really thought much about neutrophils. That is until recently, when I learned about Neutrophil Extracellular Traps (NETs). It turns out that neutrophils are pretty awesome, sacrificing themselves in a cloud-like explosion of DNA, chromatin, and granule proteins
to produce mesh-like extracellular traps that, when fully hydrated, are 10–15X larger than the volume of cells from which they were generated (4). NETs have a couple of functions. First they trap invading microbes, which stick to the NET filaments mostly via charge interactions. Pathogens trapped in this manner can range from a small bacterial cell to pathogens too large for phagocytosis, like Aspergillus. Second the NETs serve as a scaffold for clotting.
![Direct anti-microbial mechanisms from neutrophils and the Group A Streptococci counterattack. Neutrophils are equipped with multiple anti-infective strategies including the bacterial uptake (phagocytosis), the phagolysosomal degradation of bacteria via reactive oxygen species (oxidative burst), the release of antimicrobial molecules (degranulation), and the formation of a web-like structure composed of chromatin, histones, and antimicrobials (neutrophil extracellular traps [NETs]). Figure Credit: 12. Döhmann, S., Cole, J.N. and Nizet, V. (2016) Conquering neutrophils. PLOS Pathogens](https://www.promegaconnections.com/wp-content/uploads/2017/01/journal.ppat_.1005682.g001-1024x704.jpg)
NETs are formed through a special process of cell death described as NETosis which is characterized by loss of integrity of intracellular membranes followed by compromise of the plasma membrane. NETosis can be triggered by pathogen-associated molecules such as LPS or by endogenously produced signals such as ROS or platelets activated via Toll-like receptor 4.
During NETosis the neutrophils flatten and attach to the substrate. Their nuclei lose the lobules and chromatin decondenses. The inner and outer membranes of the nuclear envelope detach and the cytoplasmic granules disintegrate. Eventually the nuclear envelope will break into vesicles, and the cells will round up and contract until the plasma membrane ruptures and the interior contents of the cell are spewed into the extracellular environment. The result is the formation of the mesh-like NETs that consist of 17nm filaments composed of stacked nucleosomes and studded with granular proteins (4).
An Ancient Process Conserved across Evolution
Just as weaving is truly an ancient art, dating back to the Paleolithic era, the use of DNA and histones as part of the innate immune response is ancient biology. Mammalian neutrophils are not the only cells that respond to immune threats by weaving traps. Eosinophils and mast cells in mammals and other types of granulocytes in non-mammalian vertebrates also can create extracellular meshes composed of DNA and protein in response to disease or damaged tissues (4). Plants also exhibit a similar defense mechanism. In a 2010 review article Hawes and colleagues describe work in plants that suggests root tip border cells may function in a similar manner to protect the plant to create root extracellular traps (8,9). These cells rapidly synthesize and produce extracellular DNA in response to challenge with fungal pathogens, and histone H4 is among the more than the 100 proteins associated with the root cap “secretome” (8,9).
Not only are extracellular traps incorporating DNA and histones evolutionarily conserved, but they can also drive evolution because they put selective pressure on pathogens with traits that allow them to “escape” traps. For instance M1 strains of Group A Streptocooci (GAS) express a DNase that allows them degrade NETs (10–12).
When Warp and Weft Aren’t Right
Just like the warp and weft of any tapestry must be pulled to exactly the correct tension and threads placed in the right places and precisely organized in order to create a beautiful, functional fabric, the elegant innate immune response of the NET becomes ugly, full of holes and problematic for the host if not executed in the right place at the right time.
NETs and Pulmonary Disease
In the lungs over production of NETs can have significant consequences as the presence of DNA in the NETs expand dramatically in lungs, damaging alveoli. Additionally, many of the molecules of the NETs are toxic (histones, neutrophil elastase, myeloperoxidase, defensins) and can induce epithelial cell death. Cystic fibrosis patients face frequent lung infections as a result of the thickened mucus produced by their lungs. These infections trigger the production of NETs, and Net-associated proteins has been detected in the sputum of CF patients. Furthermore, CF patients who showed poorer lung function tended to have increased cell-free DNA in their airway fluid (4, 13).
Does your research involve isolating circulating cell-free DNA (ccfDNA)? Check out our applications notes for isolating cell-free DNA from a variety of sample types.
Although asthma is really a collection of diseases that result from a variety of genetic changes and environmental factors, some evidence is accumulating that NETs may play a role in particularly severe asthma that does not respond to glucocorticoid treatment (13). Both eosinophil and neutrophil extracellular traps have been detected in patients with neutrophilic asthma, and there is some suggestion that DNase treatment in asthmatic mice improves lung resistance and decreases oxidative stress.
NETs and Autoimmune Diseases
Systemic lupus erythematosus (SLE) is an automimmune disease in which patients often make antibodies against DNA, histones and neutrophil proteins. Some studies suggest that neutrophils isolated from SLE patients are primed to make NETs (4). Several studies have shown that SLE patients exhibit increased levels of circulating cell-free DNA in their plasma (possibly due to increased NETs), and at least one study suggests that monitoring the levels of this cell-free DNA could be useful in diagnosis (4, 14). Enhanced NET formation has also been linked to rheumatoid arthritis, and studies suggest that screening sera from patients for proteins and other molecules associated with NET formation could be useful for diagnosis of RA (14).
NETs and Trauma and Injury
NETs promote clot formation in response to injury, reducing blood loss and preventing the spread of bacteria. However, in excess they can stop critical blood supply to organs causing ischemia, and may result in further damage after an initial cardio vascular event (6). One small clinical study suggests that evaluating the circulating cf-DNA/NETs in emergency patients with multiple trauma may be predictive of the occurrence of sepsis or an inflammatory “second hit” after initial treatment (5). Similarly, NETs formed too closely with the outermost layer of the placenta may be involved in some of the symptoms of pre-eclampsia in pregnancy, particularly hypoxia of the fetus (4).
Summary
The formation of NETs as part of the innate immune response is amazing biology. As we continue to improve our ability to detect circulating cell-free DNA and NETs, we will learn more about biological events in which NETs are involved; we may even discover new ways that cell-free DNA is generated. Not only will we learn about human immunology and disease, but we will also begin to weave a larger picture of the evolution of living systems and the mechanisms that have developed to protect the genetic material and ensure its passage from generation to generation.
Literature Cited
- Jiang, P. and Lo, Y.M.D. (2016) The long and short of circulating cell-free DNA and the ins and outs of molecular diagnostics. Trends in Genetics 32, 360–371.
- Burke, E. (2014) Circulating Tumor DNA: A new generation of cancer biomarker. NHGRI Genome Advance of the Month [Internet: https://www.genome.gov/circulating-tumor-dna-a-new-generation-of-cancer-biomarkers Accesed January 12, 2016]
- Karachaliou, N. et al. (2015) Real-time liquid biopsies become a reality in cancer treatment. Ann Med. 3, 36.
- Brinkmann, V. and Zychlinsky, A. (2012) Neutrophil extracellular traps: Is immunity the second function of chromatin? Cell Biol. 198, 773–83.
- Sterfan, M. et al. (2008) Neutrophil –derived circulating free DNA (cf-DNA/NETs): A potential prognostic marker for post-traumatic development of inflammatory second hit and sepsis. SHOCK 30, 352–8.
- Miyata, T. and Fan, X. (2012) A second hit for TMA. Blood 120, 1152–4.
- Brietbach, S., Tug, S. Simon P. (2012) Circulating cell-free DNA: An up-coming molecular marker in exercise physiology. Sports Medicine 42, 565–86.
- Hawes, M.C. et al. (2011) Extracellular DNA: The tip of root defenses? Plant Sci. 180, 741–5.
- Driouich, A. et al. (2013) Root border cells and secretions as critical elements in plant host defense. 16, 4890–95.
- Buchanan, J.T. et al. (2006) DNase expression allows the pathogen Group A Streptococcus to escape killing in neutrophil extracellular traps. Current Biology 16, 396–400.
- Walker, M. et al. (2007) DNase Sda1 provides selection pressure for a switch to invasive group A streptococcal infection. Med. 13, 981–5.
- Döhmann, S., Cole, J.N. and Nizet, V. (2016) Conquering neutrophils. PLOS Pathogens. July 28.
- Nery Porto, B. and Stein, R.T. (2016) Neutrophil extracellular traps in pulmonary diseases: Too much of a good thing? Frontiers in Immunology 7, 311.
- Hendy, O.M. et al. (2016) Circulating cell free DNA as a predictor of systemic lupus erythematosus severity and monitoring of therapy. Egyptian J. Med. Hum. Gen. 17, 79–85.
- Chowdhury, C.S. et al. (2014) Enhanced neutrophil extracellular trap generation in rheumatoid arthritis: Analysis of underlying signal transduction pathways and potential diagnostic utility. Arthritis Res. Ther. 16, R122.
Michele Arduengo
Latest posts by Michele Arduengo (see all)
- An Unexpected Role for RNA Methylation in Mitosis Leads to New Understanding of Neurodevelopmental Disorders - March 27, 2025
- Unlocking the Secrets of ADP-Ribosylation with Arg-C Ultra Protease, a Key Enzyme for Studying Ester-Linked Protein Modifications - November 13, 2024
- Exploring the Respiratory Virus Landscape: Pre-Pandemic Data and Pandemic Preparedness - October 29, 2024
