Rectal cancer cases are rising in young adults (1). Typically, these cancers are treated with a multipronged approach that includes chemotherapy, radiation and surgery. These treatments show complete response in approximately 25% of patients and come with a long list of toxic side effects and life-altering complications including negative effects on bladder and bowel function, sexual health and fertility issues (2).
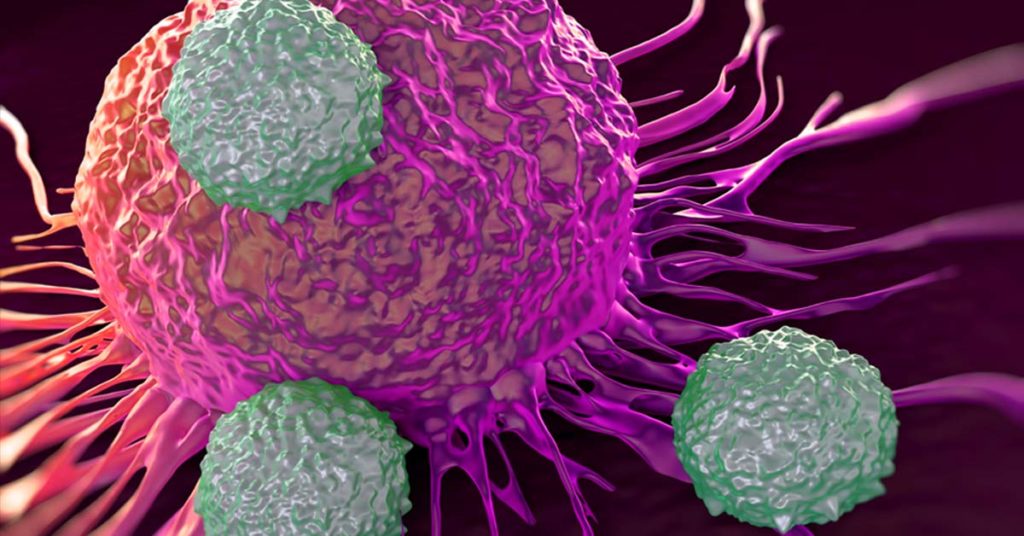
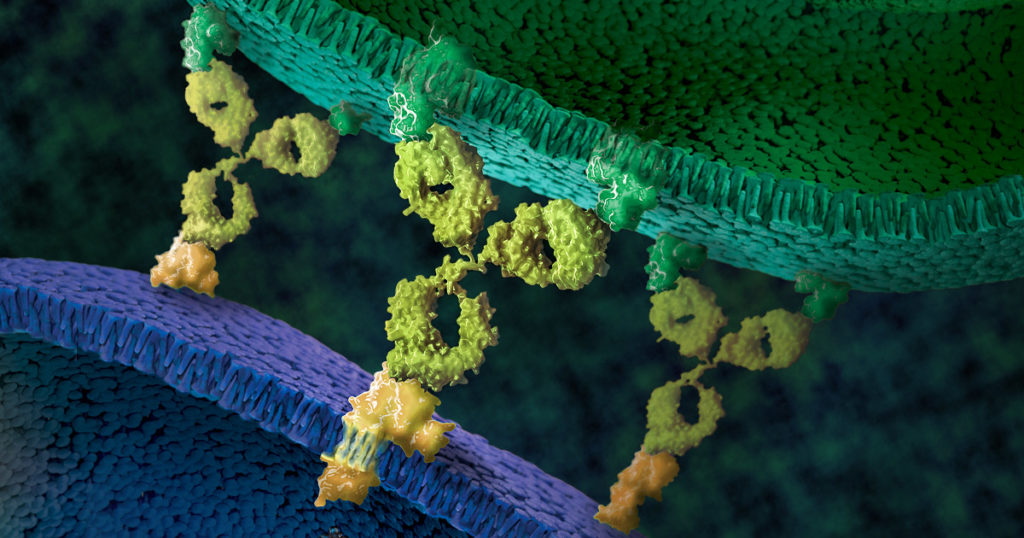
Approximately 5–10% of rectal cancers have deficiencies in their mismatch repair mechanisms (dMMR), and these cancers tend to be less responsive to standard chemotherapy treatments (2). Tumors are identified as dMMR using either immunohistochemistry (IHC) to detect the presence or absence of the major mismatch repair proteins, or by molecular testing for high-frequency microsatellite instability (MSI-H), the functional evidence of dMMR . These tumors often have somatic mutations that produce “foreign” proteins that can be detected by the immune system. As a result, these tumors are effective at priming an immune response and tend to respond well to immune checkpoint therapies such as PD-1 blockade treatments. Immune checkpoint blockade, or immune checkpoint inhibitor, therapies are a revolutionary, and relatively new, approach to treating cancer. Some tumors express immune checkpoints to prevent the immune system from producing a strong enough immune response to kill the cancer cells. Immune checkpoint blockade therapies work by blocking immune checkpoint proteins that act to negatively regulate the immune system through the PD-1 pathway. When these checkpoint proteins are blocked, the body’s T-cells can recognize and kill the cancer cells.
Continue reading “PD-1 Blockade Treatment shows 100% Tumor Resolution in Mismatch Repair Deficient Rectal Cancer Patients”