Antibiotic-resistant bacteria and their potential to cause epidemics with no viable treatment options have been in the news a lot. These “superbugs,” which have acquired genes giving them resistance to common and so-called “last resort” antibiotics, are a huge concern as effective treatment options dwindle. Less attention has been given to an infection that is not just impervious to antibiotics, but is actually enabled by them.
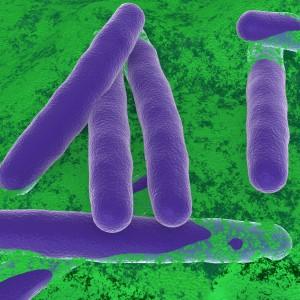
Clostridium difficile Infection (CDI) is one of the most common healthcare-associated infections and a significant global healthcare problem. Clostridium difficile (C. diff), a Gram-positive anaerobic bacterium, is the source of the infection. C. diff spores are very resilient to environmental stressors, such as pH, temperature and even antibiotics, and can be found pretty much everywhere around us, including on most of the food we eat. Ingesting the spores does not usually lead to infection inside the body without also being exposed to antibiotics.
Individuals taking antibiotics are 7-10 times more likely to acquire a CDI. Antibiotics disrupt the normal flora of the intestine, allowing C. diff to compete for resources and flourish. Once exposed to the anaerobic conditions of the human gut, these spores germinate into active cells that embed into the tissue lining the colon. The bacteria are then able to produce the toxins that can cause disease and result in severe damage, or even death.
Continue reading “Shining Light on a Superbug: Clostridium difficile”