Alzheimer’s disease is a devastating, progressive degenerative brain condition that starts with mild dementia symptoms like memory issues and gradually worsens to the point where you can no longer communicate or care for yourself. For anyone with personal experience with it, Alzheimer’s looms like a specter over the natural process of aging.
In the beginning phase of Alzheimer’s, abnormal plaques of the protein, amyloid-β, develop. These protein clumps can accumulate for decades with no detectable impact on cognitive ability or brain health. Eventually, a second protein, tau, begins to gather and form intercellular, fibrous, tangles. It is with the formation of these tau tangles that symptoms first appear. The combined presence of these extracellular plaques and intercellular tangles are the hallmarks of Alzheimer’s disease.
Exploring the Immune System’s Role in Disease Development and Progression
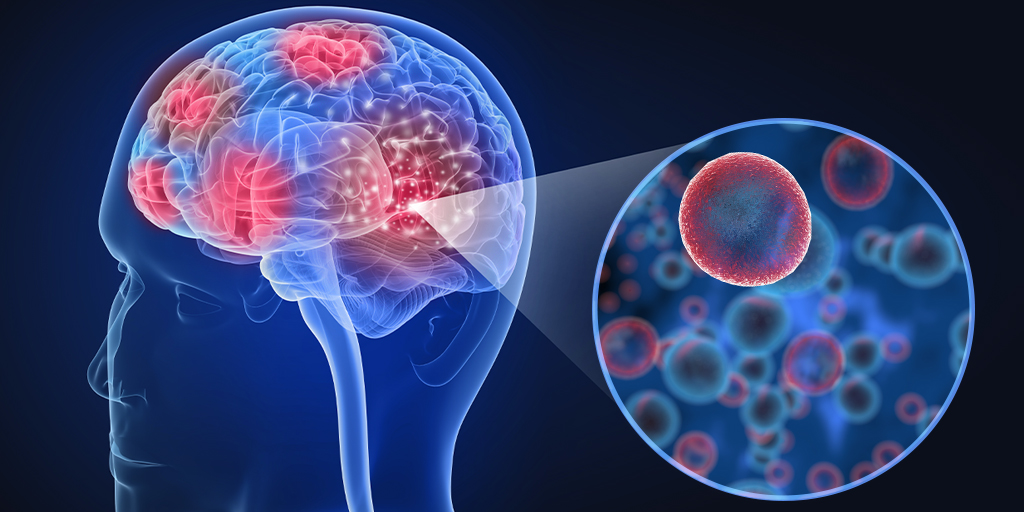
Although scientists are still working to unravel the complex changes in the brain that are involved with developing this disease, we do know neuroinflammation is found in the brains of people with Alzheimer’s, suggesting an immune response is triggered. For this reason, the role of the immune system in driving brain damage is a growing focus area for researchers. One important component of the brain’s innate immune response are microglia, the brain’s resident immune cells. Microglia are known to become activated and dysfunctional as amyloid plaques build up, and this dysfunction only worsens as tau tangles form.
Recently researchers at Washington University School of Medicine turned their attention to investigating what role a different type of immune cell, the T cell, might play in neurodegeneration and, thus, disease progression (1). To do this, the researchers used four different mice strains in their study. Two strains developed amyloid plaques but not neurodegeneration, a third strain developed tau tangles and subsequent brain atrophy, and the third strain did not develop plaques or tangles and showed no impairment. By comparing the immunological cell makeup in the brains of the different mice strains they discovered that the brains of mice with tau tangles contained a larger number of T cells compared to the other strains. The T cells were found in the highest numbers in the areas of the brain where microglia were most concentrated and the most degeneration has occurred.
T cells and Microglia Drive Neurodegeneration
The study showed that the two immune cells work together, creating an inflammatory response cycle that drives neuronal damage. Microglia function to attract and activate T cells in the brain. These T cells then drive microglia towards a higher inflammatory state, which in turn attracts more T cells.
The researchers further found that Interrupting this immune response cycle reduced neuronal damage in the brain. Using antibodies to limit T cells from entering the brains of mice with the tau tangles they showed that there were a lower number of inflammatory microglia in their brains, and these mice developed less neurodegeneration and atrophy, and showed improved cognitive function.
Much of the current Alzheimer’s research targets microglia or tau protein tangles. The implication of T cells in neurodegenerative disease progression offers another potential therapeutic target. This is only the beginning, however. There are still a lot of questions to be answered around what signaling pathways are used by the microglia and T cells to interact and produce these toxic results. While hopefully understanding these triggers could lead to promising new therapeutic treatments, that day is still much too far away for the millions of Alzheimer’s patients and their families.
Reference
- Chen, X. et al. (2023) Nature, March 8. doi: 10.1038/s41586-023-05788-0.
