Imagine driving in your car and suddenly not recognizing where you were going and having no idea how to find your way home. What if you looked across the breakfast table at your spouse and no longer recognized them? Or maybe you have to brace yourself every time you visit your parent, waiting for the day when they won’t know who you are. This is the reality for the estimated 50 million (worldwide) Alzheimer’s disease sufferers and their families.
In a world with an aging population, Alzheimer’s is a growing problem. Recent estimates suggest that 11% of people over the age of 65 have Alzheimer’s disease. For people 85 and older, that number increases to 32% (1).
Alzheimer’s disease is a devastating degenerative brain disease. It is the most common cause of dementia and is characterized by a decline in cognitive skills such as memory, language skills, communication and problem-solving abilities. These symptoms make it difficult for people with Alzheimer’s to perform everyday activities. It also is difficult to diagnose, even more, difficult to treat, and, as of now, impossible to cure.
Tangles and Plaques
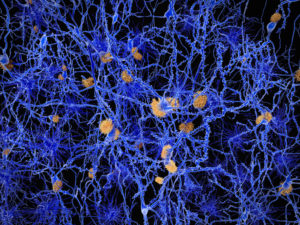
Clinically, Alzheimer’s disease is characterized by the development of one of two types of lesions: neurofibrillary tangles or amyloid plaques. Neurofibrillary tangles are caused by defective tau proteins and are located inside the neurons of the brain. These defective tau proteins clump together into a thick mass that causes microtubules to twist and leads to the disruption of the supply of nutrients and other materials to areas of the brain. Amyloid plaques are extracellular fibrillar deposits of amyloid-ß proteins that develop between neurons.
Opening the Blood Brain Barrier with Microbubbles and Ultrasound
A paper that came out almost two years ago offered hope for eliminating one of these two lesion types. Published in Science Translational Medicine (2), the author’s used repeated scanning ultrasound (SUS), specifically a nonthermal focused ultrasound, coupled with the injection of microbubbles (acting as ultrasound contrast agents) to transiently open the blood-brain barrier (BBB) as a way to encourage amyloid-ß clearance in the brain. Using this treatment, the researchers were able to at least partially restore memory functions and clear over half the plaques without doing damage to the surrounding brain tissues.
The principle is simple. When the microbubbles intercept the ultrasound pulses, they expand and contract through a process called acoustic cavitation. This in turn disrupts the vessel walls through dilation and contraction and results in transient openings in the blood-brain barrier. This approach has been used before to help deliver therapeutic agents across the blood-brain barrier.

Results in a Mouse Model
The author’s used as a model system a mouse strain (APP23 mice) that is characterized by the development of mature amyloid plaques mostly in the cortex as well as the associated memory deficits. For the study, the authors compared the animals that received the SUS treatment with littermates that were not treated (sham treatment).
In behavioral memory test, they found that mice that received the SUS treatment performed better in both short and long-term memory tests than the animals who received the sham treatment. Animals were sacrificed following real or sham treatment, and silver staining was used on brain sections to distinguish mature amyloid-ß plaques. In the treated animals, the cortical area occupied by plaques was reduced by 56% and the average number of plaques per section decreased by 52%. The microglia in the treated groups were more highly activated than those in the control group, suggesting that the clearing might be due to phagocytosis of amyloid-ß by the microglia.
Final Thoughts
The work sounds incredibly promising, but there are still a lot of unknowns. For one, they only used one model system, and they would need to show similar results with other amyloid-ß strains of mice as well as additional model systems. And even if the treatment worked in all mouse models, it is also unknown how well the treatment would translate to the physiology (i.e., larger brain size, thicker skull) of larger mammals.
This work also highlights part of what makes science such a fascinating field. Simply put, approaching a problem from a different angle. When people think of treatments for a disease, they assume a drug or therapeutic agent (the take a pill or get a shot approach). But scientists see things from different angles, and sometimes the solution might be something as simple and elegant tiny bubbles and ultrasound waves.
References
- Hebert LE, Weuve J, Scherr PA, Evans DA. (2013) Alzheimer disease in the United States (2010-2050) estimated using the 2010 Census. Neurology, 80, 1778–83.
- Leinenga, G and Götz, J. (2015) Scanning ultrasound removes amyloid-ß and restores memory in an Alzheimer’s disease mouse model. Sci. Transl. Med. 7, 278ra33.