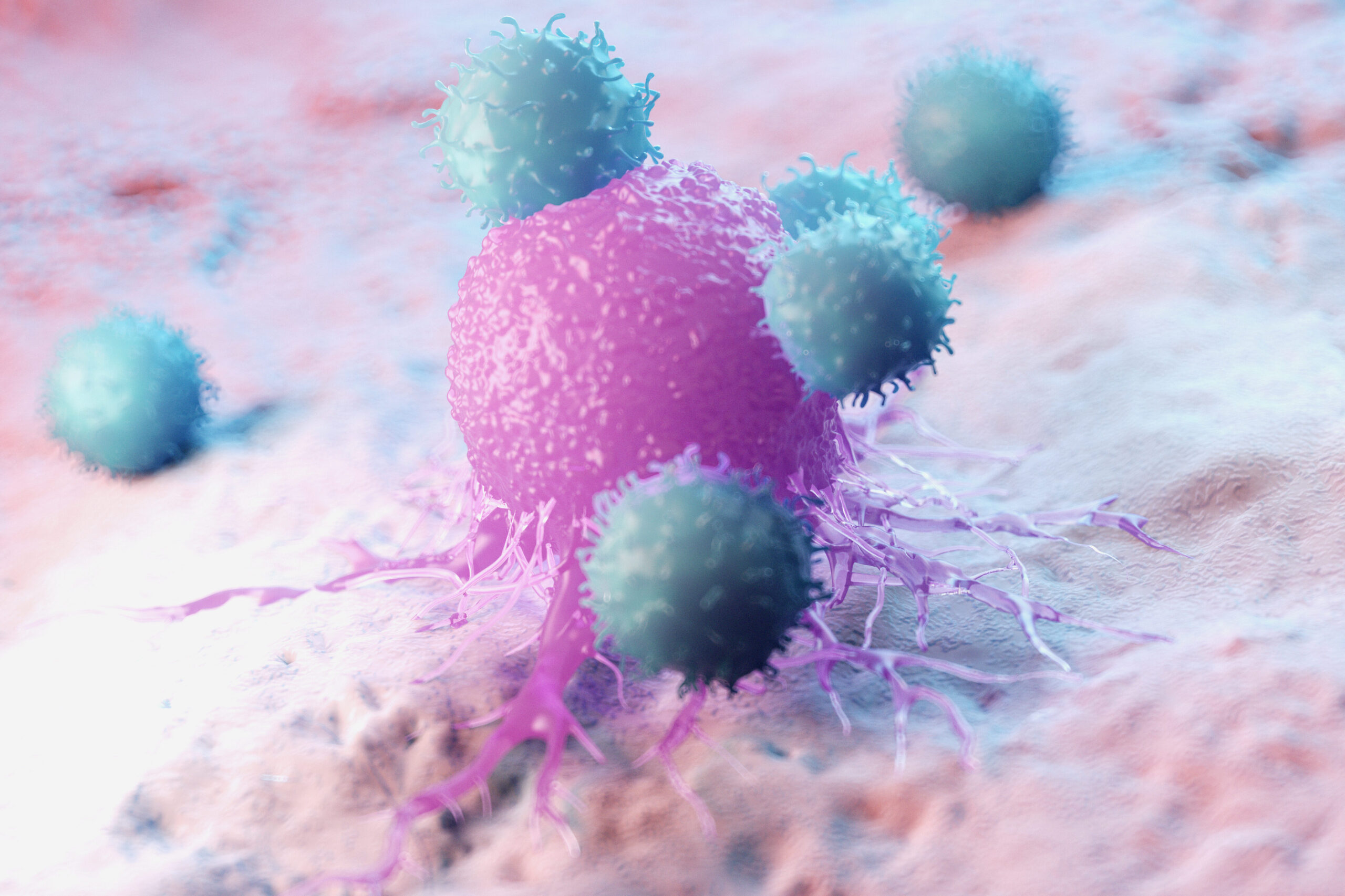
T cell-based immunotherapies, including CAR-T and TCR-T therapies, have transformed cancer treatment. T cells are a type of white blood cell that plays a central role in the immune system, recognizing and eliminating abnormal or infected cells. These therapies train T cells to attack tumors; however, a major hurdle remains: most lab-grown T cells fail to persist after an infusion in a patient. Despite transferring millions of tumor-targeting cells, many quickly die off, limiting their effectiveness inside the body. But why?
Researchers at the University of Pittsburgh have uncovered a key reason for this failure—T cells are often grown using tradition culture methods of glucose-rich media that aids in rapid T cell growth but also makes them overly dependent on that same sugar for energy. When these cells are then infused into the body, they are exposed to a nutrient-poor tumor microenvironment (TME). With little to no glucose and an inability to adapt, many of these T cells die off quickly, thereby reducing the long-term impact of the therapy. Keep reading for more information on the study:
The Problem: Lab-Grown T Cells Are Metabolically Mismatched
One of the ways T cells can be used is through adoptive cell therapy (ACT), which works by removing T cells from a patient, expanding them in the lab and reinfusing them to attack tumors. However, the way these cells are cultured does not mimic real physiological conditions, creating a metabolic mismatch:
- In vitro-expanded T cells (in lab) rely heavily on aerobic glycolysis, burning glucose rapidly to sustain growth. Traditional expansion media is glucose-heavy, making T cells reliant on sugar for energy.
- In vivo-expanded T cells (inside the body), which develop naturally in response to infections or tumors, have greater mitochondrial function, allowing them to use diverse energy sources beyond glucose.
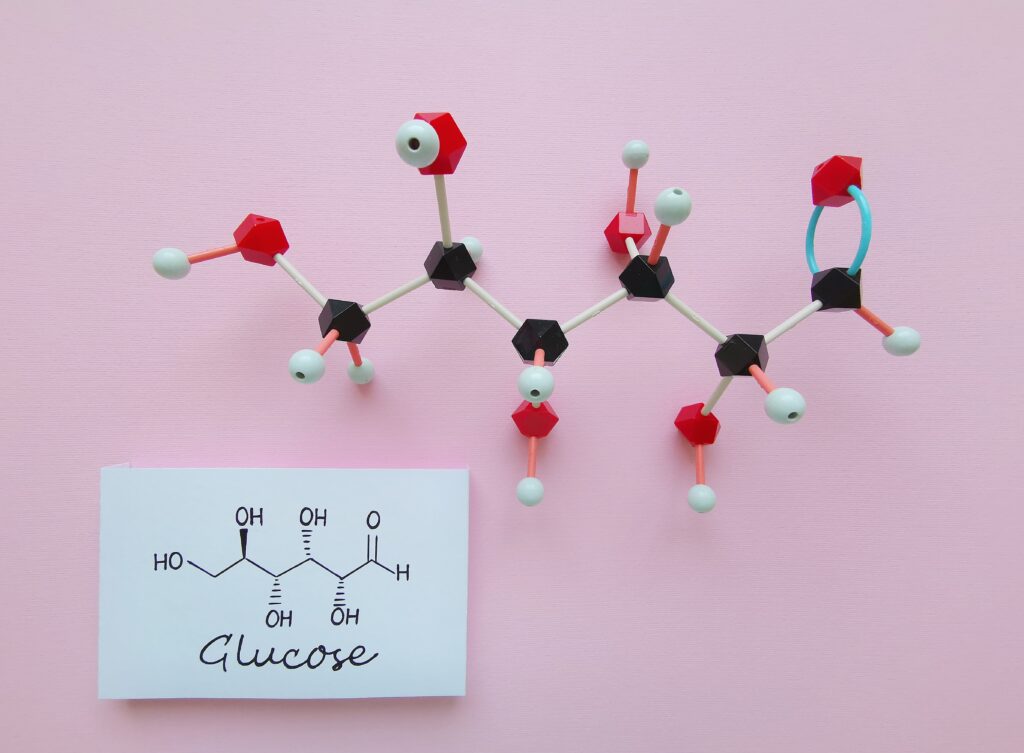
This metabolic mismatch means that while lab-grown T cells proliferate rapidly, they struggle to survive once infused into a patient. Unable to efficiently switch to alternative energy sources, these glucose-dependent cells face a nutrient-poor tumor environment, limiting their long-term persistence and effectiveness in therapy. The study’s goal was to modify T cell metabolism during expansion to better prepare them for long-term persistence inside the body.
The Breakthrough: Rewiring T Cell Metabolism with DCA
To overcome the glucose dependency of in vitro-expanded T cells, researchers hypothesized that inhibiting pyruvate dehydrogenase kinase 1 (PDHK1) with dichloroacetate (DCA) would shift T cells away from glycolysis and toward mitochondrial metabolism. This metabolic adjustment was expected to enhance their adaptability to the low-glucose tumor microenvironment (TME), improving their persistence and function after infusion.
To test this, they conducted a series of in vitro and in vivo experiments to assess whether DCA-conditioned T cells would outperform traditionally expanded ones in terms of persistence, tumor-fighting ability and epigenetic changes.
How the Study Was Conducted
Comparing In Vitro and In Vivo Expanded T Cells and Their Persistence:
- Researchers first analyzed how lab-expanded T cells differ metabolically from those naturally expanding inside a living organism. They confirmed that in vitro-expanded T cells relied far more on glycolysis, supporting the idea that traditional glucose-heavy culture conditions create metabolically fragile cells.
- To test this further, they conducted a comparative analysis of T cells expanded in standard glucose-rich media versus DCA-supplemented media, measuring metabolism, survival, and function to determine if adaptability improved.
- Mice were then infused with either DCA-treated or traditionally expanded T cells to observe differences in persistence.
- Results: DCA-treated T cells persisted significantly longer, with over 5% still circulating nearly a year later, compared to traditionally expanded T cells, which disappeared within weeks after infusion.
Evaluating Tumor-Fighting Ability and Epigenetic Changes
To further assess the efficacy of DCA-expanded T cells, mice with melanoma were treated with either DCA-conditioned or traditionally expanded T cells. Results:
- Stronger tumor control and improved survival rates.
- Increased long-term immune memory, meaning these T cells could prevent tumor recurrence
Additionally, researchers investigated epigenetic changes to gain deeper insight into why DCA-treated T cells survived longer and showed enhanced antitumor effects.
- Histone acetylation, a key epigenetic modification, was significantly increased in DCA-conditioned T cells, especially at genes linked to longevity and immune memory.
- These findings suggest that DCA doesn’t just alter metabolism—it reprograms T cells at a genetic level to promote stemness, persistence and adaptability.
Why does this matter? If metabolism-epigenetic interactions improve T cell survival, this strategy could extend beyond cancer to other immune-based therapies, such as treatments for autoimmune diseases or chronic infections, where long-lasting T cell responses are crucial.
Why does this matter?
DCA-based metabolic reprogramming provides a new way to enhance T cell therapies, addressing key challenges like persistence and adaptability.
- Improved T Cell Longevity: DCA-treated T cells remained in circulation for nearly a year, a significant improvement over standard methods.
- Stronger Tumor Control: Mice treated with DCA-conditioned T cells had better tumor clearance and survival outcomes.
- Greater Metabolic Flexibility: These cells adapted more efficiently to the body’s nutrient-limited environments, making them more resilient in tumors.
- Potential Beyond Cancer: This approach could improve other cellular therapies, including treatments for autoimmune diseases and chronic infections, where long-term T cell survival is crucial.
A Small Change with Big Potential
T cells are often called the “soldiers” of the immune system, but how they are trained in the lab determines how well they fight in the body. This study shows that by fine-tuning T cell metabolism before infusion, we can create stronger, longer-lasting immune cells that are better equipped to eliminate cancer.
If these results hold true in human trials, DCA conditioning could be a game-changer for the future of cancer immunotherapy.
References:
- Frisch, A. T., Wang, Y., Xie, B., Yang, A., Ford, B. R., Joshi, S., Kedziora, K. M., Peralta, R., Wilfahrt, D., Mullett, S. J., Spahr, K., Lontos, K., Jana, J. A., Dean, V. G., Gunn, W. G., Gelhaus, S., Poholek, A. C., Rivadeneira, D. B., & Delgoffe, G. M. (2025). Redirecting glucose flux during in vitro expansion generates epigenetically and metabolically superior T cells for cancer immunotherapy. Cell Metabolism. https://doi.org/10.1016/j.cmet.2024.12.007
- Ktori, S. (2025, January 28). Addition to T Cell Expansion Media Leads to Improved Antitumor Efficacy in Mice. GEN – Genetic Engineering and Biotechnology News. https://www.genengnews.com/topics/cancer/addition-to-t-cell-expansion-media-leads-to-improved-antitumor-efficacy-in-mice
Latest posts by Shannon Sindermann (see all)
- What 32,000 3D Spheroids Revealed About Culture Conditions - April 15, 2025
- Can Fungi Help Clean Up Environmental Contaminants? - March 20, 2025
- Reprogramming T Cells with DCA: A Metabolic Breakthrough - February 7, 2025
