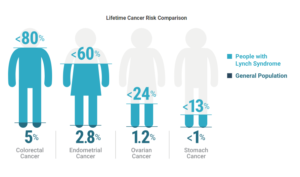
Lynch Syndrome is a hereditary condition caused by germline mutations that inactivate at least one of the major DNA mismatch repair (MMR) genes. Individuals with Lynch Syndrome have an elevated risk of developing several cancers, especially colorectal, uterine and endometrial. Approximately 1 in 279 individuals in the United States is Lynch-positive, but most people are unaware of their status.
Lynch Syndrome can be diagnosed following screening by microsatellite instability (MSI) analysis or immunohistochemistry (IHC) for the MMR proteins. For some patients, MMR gene sequencing is as easy as an oral “swish.” However, the genetic basis of Lynch Syndrome and its clinical relevancy are relatively recent discoveries. Long before modern sequencing methods simplified testing and diagnosis, a seamstress in Ann Arbor, Michigan correctly predicted her own Lynch Syndrome status based only on her family history. Talking with Dr. Alfred Scott Warthin in the late 19th century, she said that since so many of her family members had died of several specific cancers, she believed that she would follow the same path. Several years later, she unfortunately proved herself right.
Dr. Warthin took interest in the story and began studying the woman’s family. At the time of their conversation, five of her nine siblings had already been diagnosed with uterine, stomach or “abdominal” cancer. Warthin concluded that the family, which he dubbed “Cancer Family G,” did, in fact, have a predisposition to cancer. Warthin and other researchers continued studying the family for several decades. They found that cancers of the colon, uterus and stomach were most common, and that many members of the family were diagnosed at extraordinarily young ages.
In the 1970s, Dr. Henry T. Lynch organized a family reunion for Cancer Family G and subsequently published a report on “Cancer Family Syndrome.” By this time, 95 members of the family had developed one of the expected cancers. Dr. Lynch still didn’t have the technology to determine the molecular basis of the disease, but he noticed that it followed an autosomal dominant inheritance pattern.
In the mid-1990s, three labs simultaneously discovered microsatellite instability and its connection to colorectal cancer. It had been established in bacteria and yeast that inactivating mutations in DNA mismatch repair genes resulted in mutations in microsatellite sequences, so several labs began racing to clone the human homologs of the DNA MMR genes. Within a few months, two labs had cloned the MSH2 gene and found mutations that were present in members of Lynch-positive families who developed cancer.
Around this time, the name “Lynch Syndrome” was adopted to apply to families carrying germline mutations in a gene associated with the condition. Further research established four genes (MSH2, MLH1, MSH6, PMS2) as “Lynch Syndrome Genes,” and researchers began working on guidelines for diagnostic testing (See “The History of Lynch Syndrome” below for further reading).
Today, over two decades later, many researchers are pushing for the adoption of universal tumor screening for Lynch Syndrome. One of the widely recommended screening method is MSI analysis. MSI-H status indicates that certain sections of DNA called microsatellites have become unstable because the major mismatch repair genes that correct errors during DNA replication are not functioning properly. MSI status can influence treatment decisions, based on the 2015 discovery that MSI-H tumors respond well to immunotherapy drugs (1).
Lynch Syndrome awareness is also important knowledge for a patient’s family. Lynch-associated cancers are among the most preventable, so individuals who know they are Lynch-positive can work with their healthcare providers to develop robust strategies for prevention and surveillance. As one Lynch-positive mother said to her Lynch-positive son, “Your knowledge is power, and it’s going to keep you healthy and safe.”
March 22, 2019 is Lynch Syndrome Awareness Day, and we’re encouraging everyone to join the fight against colorectal cancer. Visit our website to learn more about Lynch Syndrome and MSI status.
Further reading:
Life with Lynch Syndrome: Read about what a Lynch Syndrome diagnosis means for Carrie Ketcham and her family
Dreaming of Universal Tumor Screening: Learn how cancer genetic counselor Heather Hampel is advocating for universal tumor screening and more Lynch Syndrome awareness
The History of Lynch Syndrome: Dr. C. Richard Boland and Dr. Henry T. Lynch provide a broad review of Lynch Syndrome research, starting over a hundred years ago.
Learn more about Lynch Syndrome Testing and Detection at our website.
References
(1) Le, D.T. et al. (2015) PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. New Engl. J. Med. 372, 2509–20.
Latest posts by Jordan Villanueva (see all)
- Tackling Undrugged Proteins with the Promega Academic Access Program - March 4, 2025
- Academic Access to Cutting-Edge Tools Fuels Macular Degeneration Discovery - December 3, 2024
- Novel Promega Enzyme Tackles Biggest Challenge in DNA Forensics - November 7, 2024
