But the reservoir of natural products with the potential to act as antibacterial drugs has not yet been exhausted. In contrast to general thinking by drug companies, screening for such products may well still have a bright future” Nature News and Views: “Antibiotic resistance: To the rescue of old drugs” Meziane-Cherif & Courvalin, Nature 510, 477–478.
The emergence of bacteria that are resistant to antibiotics has been an object lesson in the relentlessness of natural selection; the moment a new antibiotic is developed and introduced, the countdown to the emergence of resistance begins. The race to keep the one step ahead of emerging resistance mechanisms has been going on since antibiotics were first introduced.
The history of the development of penicillin and related antibiotics is both an illustration of the ingenuity of scientists and of the never-ending nature of this battle with emerging resistance. The Nature paper is the latest installment in that story.
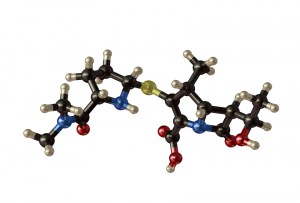
Beta-lactam antibiotics (Penicillin and its derivatives such as cephalosporins, monobactams and carbapenems) are so named because they all contain a beta-lactam ring structure. This structure is key to their mechanism of action, which is to disrupt synthesis of the bacterial cell wall. As each new generation of drugs has been introduced, resistance has faithfully followed. Resistance to beta-lactam antibiotics occurs when the target bacteria produce a beta-lactamase enzyme, which hydrolyzes and destroys the beta lactam ring structure and inactivates the antibiotic.
![Beta lactam ring structure in 1) Penicillin and 2) Cephalosporin. Image Credit: By Fvasconcellos 19:02, 23 October 2007 (UTC) (Own work) [Public domain], via Wikimedia Commons from Wikimedia Commons.](https://www.promegaconnections.com/wp-content/uploads/2014/07/500px-Beta-lactam_antibiotics_example_1.svg_-198x300.png)
One strategy to overcome this type of resistance is to continually develop new compounds that are not susceptible to the action of known beta lactamases. This has led to the development of many generations of beta-lactam antibiotics with varying structures and different tolerances to existing beta-lactamases. Use of these new variants has turn been accompanied by the eventual development of resistance to each type of drug—-usually by the emergence of new beta-lactamases. The introduction to the Nature paper makes the point that, until recently, carbapenem resistance was not a significant problem and so carbapenems have been used as a drug of last resort for multidrug-resistant enterobacterial infections. This makes the emergence of resistance an urgent problem.
A second strategy to overcome resistance is the use of combination therapies involving both an antibiotic and an inhibitor that destroys or blocks the action of the resistance mechanism. One successful example of this is the use of amoxicillin with clavulanic acid—a compound that competitively binds to the active site of the beta lactamase enzyme, preventing it from binding to and cleaving the antibiotic. Carbapenemases, beta lactamases that inactivate carbapenems and confer resistance to them, fall into two categories: serine carbapenemases, which contain serine at the active site, and metallo-carbapenemases, which contain zinc at the active site. Drugs that inhibit serine carbapenemases exist, but until now no inhibitors of metallo-carbapenemases have been identified.
The June 26 Nature paper describes isolation of a fungal compound, aspergillomarasmine, the first compound to be identified that inhibits the activity of metallo-carbapenemases. Aspergillomarasmin was identified by screening products extracted from soil microorganisms against an engineered carbapenem-resistant E. coli strain. Upon purification, aspergillomarasmine was shown to be effective in restoring the sensitivity of resistant Enterobacteriaceae, Acinetobacter and Pseudomonas species to the antibiotic. The authors went on to show that treatment with a combination of a carbapenem antibiotic and aspergillomarasmine was effective in preventing lethality in mice infected with resistant Klebsiella pneumoniae.
In their conclusion, the authors state:
In combination with a beta-lactam antibiotic such as meropenem as we show here, resistance can be overcome and antibiotic activity fully restored. AMA (or semi-synthetic derivatives) is therefore an excellent lead for an antibiotic adjuvant co-therapy to address the recent emergence of metallo-beta lactamases in the clinic.
It’s good news that there are still options like this out there, waiting to be discovered, understood and applied.
Here’s the paper:
![]() King, A., Reid-Yu, S., Wang, W., King, D., De Pascale, G., Strynadka, N., Walsh, T., Coombes, B., & Wright, G. (2014). Aspergillomarasmine A overcomes metallo-β-lactamase antibiotic resistance Nature, 510 (7506), 503-506 DOI: 10.1038/nature13445
King, A., Reid-Yu, S., Wang, W., King, D., De Pascale, G., Strynadka, N., Walsh, T., Coombes, B., & Wright, G. (2014). Aspergillomarasmine A overcomes metallo-β-lactamase antibiotic resistance Nature, 510 (7506), 503-506 DOI: 10.1038/nature13445
Isobel Maciver
Latest posts by Isobel Maciver (see all)
- 3D Cell Culture Models: Challenges for Cell-Based Assays - August 12, 2021
- Measuring Changing Metabolism in Cancer Cells - May 4, 2021
- A Quick Method for A Tailing PCR Products - July 8, 2019
