
It’s hard not to panic in the light of recent pandemic fears and the frightening possibilities conjured up by the thought of a novel flu virus with the propensity for person-to-person spread (1-3). The specter of the 1918 pandemic has raised its ugly head, and we are left feeling intensely vulnerable to an invisible and ever-changing enemy. Have science and history left us more prepared to combat this virus than those who suffered during the devastating 1918 outbreak?
Advances in scientific discovery over the last century have armed us with the ability to know our enemy on the molecular level, and although some of the implications of that knowledge are indeed frightening, continuing pursuit of knowledge of the molecular mechanisms by which the virus survives and propagates is vital to any effort to combat the threat.
It is encouraging to know that the genome of the currently circulating H1N1 strain is sequenced already, and although experts warn us that it is too early to tell what will happen, it is good to know that certain feared virulence factors present in the 1918 strain do not appear to be evident in the currently circulating strain (2). But it is the propensity for flu viruses to change quickly that makes them unpredictable and dangerous (4). Seasonal flu is caused predominantly by influenza A viruses, which are negative-stranded RNA viruses that have a segmented genome consisting of eight RNA segments encoding genes for eleven proteins. Two glycosylated proteins on the surface of the virus, hemagglutinin (HA) and neuraminidase (NA) are used to subtype influenza A viruses. To date, 16 HA and 9 NA subtypes have been identified. The HA glycoproteins bind to sialic acid-containing receptors on the host cell surface (4-6).
Flu viruses can undergo two types of change that enable them to evade the host immune system, antigenic drift and antigenic shift. In antigenic drift, the viral coat proteins undergo continual small changes due to point mutations, causing the continual minor antigenic changes seen from year-to-year in seasonal flu strains. Antigenic shift involves a more sudden change to a viral subtype that is not currently circulating or has not been seen before, and to which people have little or no immunity (7). If such a virus can spread efficiently from person to person, a pandemic can occur.
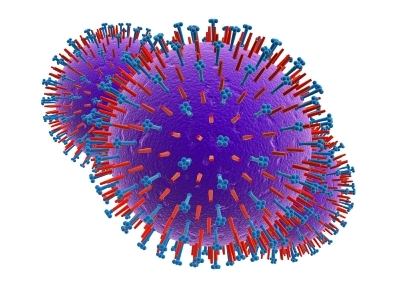
The segmented genome of influenza A viruses allows them to easily exchange genetic material. If two different viruses infect the same cell, they can exchange segments and generate offspring with many different combinations of genes. Such reassortment between an established human virus and an avian virus is thought to have resulted in the influenza strains that caused both the 1957 “Asian” flu (H2N2) and 1968 “Hong Kong” Flu (H3N2) pandemics (8). Pigs are thought to be a potentially ideal vessel in which this type of reassortment could occur, because they have receptors for both human and avian influenza viruses. This means that pig cells may be able to host both avian and human type viruses, which could recombine to a new virus combining the novel antigenicity and virulence of avian strains, with the ability to efficiently bind to human cellular receptors and spread easily from person to person (8,9).
Sequence analysis has shown that all eight segments present in the 1918 H1N1 strain were most closely related to avian viruses, suggesting that the 1918 pandemic was caused by an avian virus of novel origin that mutated to a form that was able to infect human cells and spread from person to person (10). The novel antigenicity of the virus could partly explain the virulence of the 1918 pandemic, since people would not have been previously exposed and would have had no immunity. Genetic analysis of archival samples from soldiers who died of flu revealed that the H1 glycoprotein of this strain was not only antigenically novel, but also had a mutation that allowed it to bind extremely efficiently to human cells, conferring devastating efficiency in spreading from person to person (10,11).
Since outbreaks of the H5N1 strain of avian flu in 1997 and 2004, the concern has been that such a novel avian strain will either mutate or undergo reassortment with a human strain in such a way that it gains the ability to spread easily from person to person. The “swine flu” that is the subject of current fears appears to be a reassortant containing genes from swine, avian and human influenza viruses (3).
Time will tell whether the current H1N1 strain adapts to become more virulent. Maybe another flu pandemic has arrived, maybe not, however thanks to the dedicated research and detective work of virologists, epidemiologists, and molecular biologists over the last 50 years, we are armed with more knowledge than ever before, and we surely must be in a better position to engage in the battle.
- WHO statement: May 4, 2009, H1N1 influenza situation
- Centers for Disease Control and Prevention Press Briefing, May 1, 2009.
- Cohen J., and Enserink, M. Science News: 1 May 2009 Science 324, 572 – 573.
- Reid, A. and Taubenberger, J.K. (2003) J. Gen. Virol. 84, 2285–92. PubMed.
- Lamb, R. and Krug, R. (2001) In Fields Virology, 4th Ed., pp. 1487–1531. Knipe, D. and Howley, P. Philadelphia: Lippincott Williams & Wilkins.
- White, J.M. et al. (1997). In Structural Biology of Viruses. Chiu, W., Burnett, R.M., and Garcea, R.L., editors. Oxford University Press, NY. pp80-104.
- Rambaut, A. et al. (2008) Nature 453, 615-619: PubMed.
- Howard Hughes Medical Institute Research News, May 1, 2009.
- Van Reeth, K., Nicoll, A. (2009) Euro Surveill. 14(7), 19124.
- Taubenberger, J.K., and Morens, D.M. (2006) Emerg. Infect. Dis. 12, 15–22. PubMed.
- Reid A.H., et al. (2003) Emerg Infect Dis. 9, 1249–53. PubMed.
Isobel Maciver
Latest posts by Isobel Maciver (see all)
- 3D Cell Culture Models: Challenges for Cell-Based Assays - August 12, 2021
- Measuring Changing Metabolism in Cancer Cells - May 4, 2021
- A Quick Method for A Tailing PCR Products - July 8, 2019
