In 1921, at age 39, Franklin D. Roosevelt, the man who would later be elected the 32nd president of the United States, was diagnosed with polio (poliomyelitis). His symptoms included fever, gastrointestinal issues, numbness, and leg and facial paralysis. The disease left him paralyzed from the waist down, relying on a wheelchair and leg braces to walk.

At the height of the polio epidemic in 1952, more than 3,000 people died of polio in the United States, and 20,000 more people suffered paralysis. Pictures of the era show children in special hospital wards, inside ominous-looking iron lungs, while “recovered” children played on the grounds of hospitals wearing leg braces.
In 1938, Roosevelt founded the March of Dimes, which funded the development of the Salk polio vaccine. Two years after the introduction of the Salk vaccine in 1955, polio cases in the US dropped by 90%. In fact, sustained polio transmission has been absent from the US for nearly 40 years; according to the CDC, the last case of wild poliovirus in the US occurred in 1979.
That changed in June 2022 when an adult male in Rockland County, New York, presented with fever, weakness and paralysis. A diagnosis of poliomyelitis was confirmed in July, and testing of 260 samples collected from wastewater treatment plants for SARS-CoV-2 sampling, revealed 21 samples that were positive for poliovirus. Twenty of the specimens from wastewater samples collected during May, June and July were genetically linked to the virus from the patient’s stool samples. So, for the first time in nearly 40 years, there is a documented sustained spread of poliovirus in the US. Furthermore, genetic analysis also indicates that the US case is linked to vaccine-derived viruses recently detected in Jerusalem and London.
What Is Poliovirus?
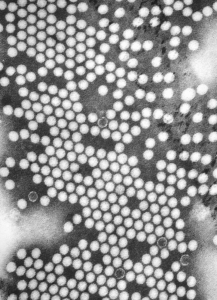
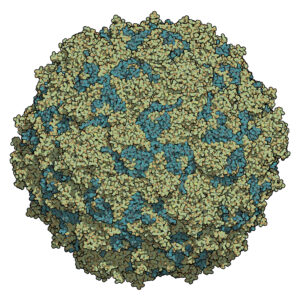
Poliovirus is a member of the Enterovirus genus of viruses. Enteroviruses are viruses that are found, at least transiently, in the gastrointestinal tract, and they are transmitted by the oral-fecal route. Enteroviruses are small viruses consisting of a positive single-stranded RNA genome and an unenveloped protein capsid that forms an icosahedron. There are three poliovirus serotypes (PV1, PV2, and PV3). Immunity to one serotype does not result in immunity to the other two. Individuals must be vaccinated against all three serotypes. Polio infects only humans, and infection is more common among children than adults.
How Did Poliovirus Re-emerge in the West and in New York?
Several factors led to the re-emergence of polio in the West. In the US, vaccination rates for polio are around 90%, which makes the risk of polio transmission very low. However, there are pockets where vaccination rates are significantly lower. Rockland County in New York is one of these places. These pockets of undervaccination are vulnerable to outbreaks of infectious diseases that are rare in communities where vaccination rates are high. Also, over the past 2.5 years, routine immunizations have been slowed by lockdowns from the COVID-19 pandemic as well as by the increased politicization of vaccination and public health care. In fact, UNICEF reported the largest sustained decline in vaccination worldwide between 2019 and 2021 in 30 years.
Nearly 70% of polio infections are asymptomatic. Often, by the time a single case involving paralysis is diagnosed, anywhere from 100 to 1,000 other individuals may have been infected. In the case from Rockland County, New York, the patient presented in June 2022 but was not officially diagnosed until nearly a month later. During this time, he was shedding virus in his stool and from his nose and pharynx, potentially infecting other individuals.
In 1988, the Global Polio Eradication Initiative was launched. Since the poliovirus infects only humans, a worldwide vaccination and monitoring program should be able to eliminate the virus. Currently, wild poliovirus is endemic only in two countries: Pakistan and Afghanistan. Polio vaccines are highly effective, and the availability of an oral vaccine that is easy to administer (no shots) and inexpensive to produce and store, means that vaccination in developing countries and remote regions of the globe is achievable. The vaccine used in many parts of the world is the oral vaccine that contains attenuated (weakened) live poliovirus. This attenuated virus can be shed by vaccinated individuals, and if it remains attenuated, can spread immunity to unvaccinated individuals. While these are all positives for the oral vaccine, the vaccine does have some risk. The shed attenuated virus could undergo genetic changes that restore its ability to cause severe infections. In these cases, unvaccinated individuals could become ill from Vaccine-Derived Poliovirus (VDPV). In fact, in the Rockland County case, the virus that infected the patient was shown by molecular analysis to be a vaccine-derived virus, derived from the PV2 serotype of the virus. Thus, there was a transmission chain from someone who had received the oral vaccine. However the chain of transmission will be virtually impossible to trace, because molecular analysis shows that the VDPV2 strain that infected the patient in Rockland county contains genetic changes that suggest that it may have been circulating for up to a year.

The Rockland case indicating a chain of transmission of VDPV2 is significant because of a decision made by global health authorities in 2016 to remove the PV2 serotype from the oral vaccine. In 2015, the wild PV2 serotype was declared eradicated. However, anyone receiving the 2016 and later vaccine would be susceptible to VDPV2 because that serotype was no longer included in the oral vaccine. In most parts of the world, this was not an issue, but in parts of Africa and Asia, VDPV2 infections are surfacing.
The US relies on a killed virus for vaccination, and because of this and the >90% vaccination rates within the population, vaccine-derived infections are not usually a problem in communities in the US. It also means that the United States was not actively monitoring for polio outbreaks through any systemic means, such as wastewater monitoring programs. Other countries are monitoring wastewater to detect the spread of polio in their communities. The United Kingdom has been monitoring since 2016, and their efforts did detect a potential virus outbreak before any cases of paralysis had presented. They immediately began a campaign to vaccinate children under five who had not been fully vaccinated to prevent an outbreak. Israel has been monitoring wastewater for the virus since 1989, and in 2013 they were able to detect and prevent an outbreak of wild polio.
The Advantages of Systemic Monitoring Using Wastewater Surveillance
Wastewater testing for SARS-CoV-2 to track and predict waves in the COVID-19 pandemic has brought wastewater monitoring for infectious disease to the forefront, providing opportunities and funding to improve the testing process and conduct routine testing. Wastewater monitoring for infectious disease outbreaks is particularly useful for tracing the spread of infectious diseases that can be asymptomatic in a majority of cases. Additionally, because these methods are based on molecular techniques such as qPCR or nucleic acid sequencing, they can be quickly modified to detect emerging pathogens. Also, often a single sample can be used to test for multiple pathogens at once. Being able to detect the presence of infectious organisms in communities before symptoms and diagnosis can better inform public health measures and local health-care providers.
Learn how wastewater monitoring has helped public health officials better understand the COVID-19 pandemic.
Wastewater-based surveillance is a public health tool that has proven its value in many instances and continues to bring value to monitoring infectious disease outbreaks. Several countries like Israel have been using wastewater-based surveillance to contain outbreaks of polio and Hepatitis A within their regions before the COVID-19 epidemic. The New York State Department of Health and the New York City Department of Health and Mental Hygiene began using wastewater monitoring to track poliovirus in July. The Sewer Coronavirus Alert Network, which is a collaboration out of Emory University in Atlanta, GA and Stanford University in California, have started daily monitoring in California wastewater plants for SARS-CoV-2, Respiratory Syncytial Virus, and Monkeypox.
From Extraction to Detection: Wastewater Surveillance Products from Promega
Our Wizard and Maxwell RSC Enivro TNA kits for the concentration and extraction of TNA from wastewater samples and the GoTaq Enviro qPCR systems provide a convenient, reliable detection method for the organism of choice.
References
Anthes, E. (2002) Polio May Have Been Spreading in New York Since April. New York Times Aug 16.
Branswell, H. (2022) U.S. Polio Case Tied to Viruses Detected in U.K., Israel, Suggesting Silent Spread. STAT News July 29.
Branswell, H. (2019) “The Switch Was Supposed to Be a Major Step Toward Eradicating Polio. Now It’s a Quandary. STAT News Sept. 13
Centers for Disease Control (2022) Poliomyelitis: For Healthcare Providers
Fields, R. (2022) How Polio Crept Back Into the U.S. ProPublica July 26. Internet: Accessed Sept. 6, 2022.
Link-Gelles, R. et al (2022) Public Health Response to a Case of Paralytic Poliomyelitis in an Unvaccinated Person and Detection of Poliovirus in Wastewater —New York , June–August, 2002 Morbidity and Mortality Weekly Report August 19 71:1065-68.
Michele Arduengo
Latest posts by Michele Arduengo (see all)
- An Unexpected Role for RNA Methylation in Mitosis Leads to New Understanding of Neurodevelopmental Disorders - March 27, 2025
- Unlocking the Secrets of ADP-Ribosylation with Arg-C Ultra Protease, a Key Enzyme for Studying Ester-Linked Protein Modifications - November 13, 2024
- Exploring the Respiratory Virus Landscape: Pre-Pandemic Data and Pandemic Preparedness - October 29, 2024
