Since about 2000 we’ve learned a lot about the bacteria in our guts. We’ve learned that the right bacterial communities in our gastrointestinal system can make us feel better, think better and even help avoid obesity (1). My colleague Isobel has previously blogged about how certain gut bacteria can improve immunotherapy outcomes.
Conversely, the wrong bacteria in our guts can have negative consequences on health and cognition.
Along the way we’ve learned that gut bacterial flora can be influenced by what we eat, certain medications like antibiotics, and even stressful events. We now know that fermented foods like yogurt, sauerkraut, kombucha and that horrible-smelling stuff (kimchi) that another colleague eats are happy food for the good gut bacteria.
And you might guess that fried foods, saturated fats and certain carbohydrates can support the growth of gut bacteria that are doing us no favors when present in large quantities in our gastrointestinal system.
Reports on how food can affect our gut flora are an opportunity to change the makeup of our gut bacteria. You can change what you eat and use supplements like probiotics to augment or improve the bacteria in your gut.
But when I read the report published by Killinger et al. that simply having an appendix can be hazardous to long-term health, it was gut news less easy to digest (2).
Killinger et al. built on a body of research regarding the business conducted by the appendix—yes, it has a job—and what’s known about Parkinson’s disease. Here is an overview.
The Appendix in Health and Disease
In the late 1970s when my brother made a sudden trip from high school to the hospital with sharp lower right abdominal pain, and a ruptured appendix, it was believed that the vermiform appendix was a useless, rudimentary sac. The appendix is several centimeters in length and hangs from the cecum near the junction of the small and large intestines. For reasons not well studied at the time, the appendix sometimes became inflamed and could even rupture, and when the painful inflammation occurred the appendix was removed (3).
It wasn’t until around 2000 that the appendix became appreciated as a reservoir of good gut bacteria, useful after illness or any time the bacterial flora in the large intestine was upset, such as after a course of antibiotics or during other stressful events (3).
The appendix is additionally important for mucosal immunity, particularly extrathymic T cells and B cells. So the news about the appendix and its functions, until very recently, was mostly good (3).
Parkinson’s Disease: More than Just Motor Symptoms
While the appendix was gaining new found respect as a source of gut immune cells and helpful bacterial flora, Parkinson’s disease (PD) was gaining in pathology. Long understood to be a disease affecting motor neurons and causing progressive motor symptoms, such as tremors, loss of upper body strength and a shuffling gait, researchers and clinicians were beginning to identify nonmotor symptoms, particular GI dysfunction, in PD patients (4). Aggregates of alpha-synuclein form Lewy bodies in the neurons of the midbrain, contributing to cell death and the motor symptoms of PD (4).
Then in 2014 Gray et al. reported the presence of the protein alpha-synuclein in the appendixes of neurologically healthy people (5).
In the work cited here, Killinger et al. from 2018, Science Translational Medicine, used information from two large datasets, the Swedish National Patient Registry (SNPR) and the Parkinson’s Progression Markers Initiative (PPMI). The former covered more than 91-million person-years and the latter contained detailed information on PD diagnosis, age of onset and genetic information (2).
They also studied appendix tissue via immunohistochemistry and found the human appendix to contain pathology-associated alpha-synuclein. Additionally, they demonstrated truncated forms of alpha-synuclein in the appendix. They showed that these truncated forms can seed the formation of Lewy body-type aggregates of alpha-synuclein, the pathological form of this protein (2).
A Long Ways from There to Here?
If you imagine for a minute the appendix, near the lower end of the abdomen, a simple tube hanging from the cecum, it seems like a long way to the brain, right?
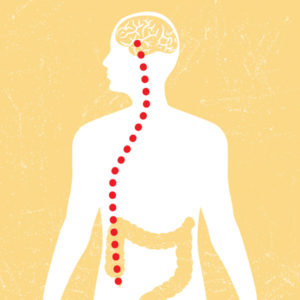
That is until you consider the vagal nerve, which runs from the lower abdomen to the midbrain, innervating tissues along its path (see illustration). Killinger et al. found abundant alpha-synuclein aggregates in submucosal and myenteric plexuses and nerve fiber of 46 of 48 individual appendixes examined. These aggregates were found in equal numbers in normal, acutely inflamed and chronically inflamed appendix tissues (2).
Other studies have shown in animals that misfolded alpha-synuclein can spread cell to cell, in prion-like fashion, triggering Lewy body-like aggregates in neurons. Procedures in which the vagal nerve connecting the GI tract to the brain is severed have been associated with lowered incidence of PD in some epidemiologic studies (2).
Additionally, alpha-synuclein aggregates have been seen in the GI tract of patients before PD diagnoses. These aggregates have demonstrated an ability to ascend the vagal nerve to the brain (2).
From their findings and those of others, Killinger et al. predicted that appendectomy would be more protective the earlier it occurred in the person’s life, and data from large epidemiologic studies supported this prediction.
It appears from the results of Killinger et al. that in addition to the role of the appendix in immunity and microbial regulation, it may also seed the gut with alpha-synuclein aggregates. The aggregates may then, through the vagal nerve, move to other tissues including the brain, potentially inducing PD pathology.
References
-
- Shreiner A.B. et al. (2015) The gut microbiome in health and disease. Curr. Opin. Gastroenterol. 31(1) 69–75.
- Killinger, B.A. et al. (2018) The vermiform appendix impacts the risk of developing Parkinson’s disease. Sci. Transl. Med. 10 eaar5280.
- Appendix Wikipedia page.
- Parkinson’s Disease Wikipedia page.
- Gray et al. (2014) Alpha-synuclein in the appendiceal mucosa of neurologically intact subjects. Mov. Disord. 29 456–63.
