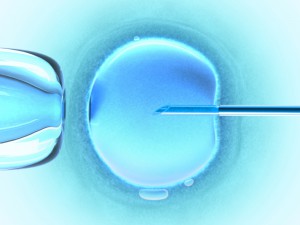
It is remarkable to me how quickly in vitro fertilization has gone from an experimental, controversial and prohibitively expensive procedure to becoming a mainstream option for those struggling with fertility issues. What was unheard of in my parents’ generation is nothing extraordinary among my friends who are having children.
My personal observations are supported by the CDC, which reported that 1.6% of all infants born in the U.S. in 2015 were the result of assisted reproductive technology (ART). This is a 33% increase since 2006, which can be attributed to rapid advances and refinements of the various technologies available to those seeking reproductive assistance.
It challenges the mind to imagine what reproductive technologies might be widespread when my children and their friends are adults. When experts speculate about the future of human reproduction, there always seems to be a lot of focus on provocative scenarios that portend a dystopian future, such as designer babies. What gets lost are some of the more general scientific advances that are being applied to ART in fascinating ways.
While improvements in reproductive technologies serve many, one group that remains underserved are pediatric cancer patients. As a result of treatment, these patients are often faced with impaired ovarian function that can prevent puberty and result in infertility. In vitro fertilization and ovarian transplants are currently used, but do not provide lasting solutions for all individuals.
In response to this need, researchers are working to develop an organ replacement that can provide long-term hormone function and fertility for all patients. A recent study in Nature Communications presented encouraging results in mice using bioprosthetic ovaries that may further revolutionize the field of ART.
Continue reading “Creating ART from 3D Printed Ovaries”