Age-related macular degeneration (AMD) is a common eye disease that can result in progressive loss of vision. While AMD typically affects older adults, a specific rare type of AMD called Malattia Leventinese/Doyne honeycomb retinal dystrophy (ML/DHRD) can appear as early as the teenage years. Although ML/DHRD is rare, its study may provide insights into broader mechanisms of retinal degeneration, which could benefit millions affected by AMD.
While the genetic cause of ML/DHRD is known, there have been no small molecule inhibitors identified that reduce the production of the disease-causing protein. However, researchers from the University of Texas Southwestern Medical Center and the University of Minnesota recently published a paper that describes a small-molecule inhibitor that addresses the primary pathology of ML/DHRD. In the paper, titled “GSK3 inhibition reduces ECM production and prevents age-related macular degeneration-like pathology,” the team used CRISPR-engineered cell lines acquired through the Promega Academic Access Program to study production of the disease-causing protein in response to treatment with inhibitors. Their results point to future strategies for developing therapeutics at the currently incurable disease.
What is ML/DHRD?
ML/DHRD is a retinal disorder that results in central vision loss. It is caused by an autosomal dominant mutation in the EFEMP1 gene. The mutation leads to misfolding of the fibulin-3 (F3) protein, which is secreted to the extracellular matrix. Accumulation of misfolded F3 disrupts the matrix and leads to deposits that damage the retina over time.
Past research has shown that knocking out F3 does not produce any retinal defects in mice or humans, and F3 removal appears to protect mice from extracellular masses that are often seen in patients with AMD. These findings suggests that knockdown of F3 could not only mitigate disease symptoms associated with ML/DHRD, but do so safely without compromising retinal integrity.
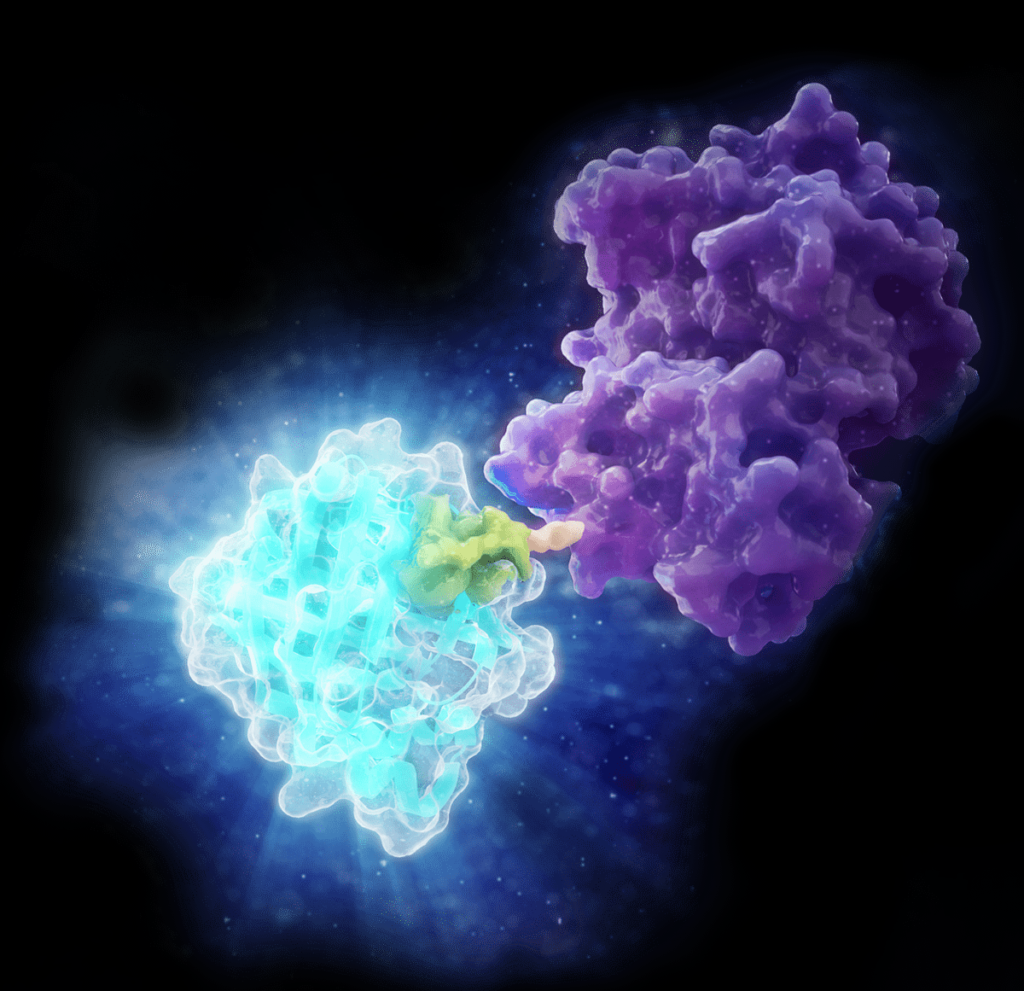
HiBiT Protein Tagging with CRISPR/Cas9
The research presented in JCI Insight was largely dependent on several cell lines in which the HiBiT protein tag was introduced immediately after the F3 signal sequence using CRISPR/Cas9. The HiBiT Protein Tagging System enables researchers to study protein function, degradation, secretion and interactions at endogenous levels. The HiBiT tag is only 11 amino acids, and when it binds to its complementation partner LgBiT, it forms the functional NanoLuc enzyme capable of producing a bioluminescent signal.
Here, the researchers employed a high-throughput screening (HTS) assay using the HiBiT cell line. They identified 127 compounds that resulted in a reduction in F3, and then further narrowed the field to 6 based on cell viability analysis and dose-response assays. Two of these compounds were identified as inhibitors of GSK3, a kinase that has been shown to regulate the production of F3 and other ECM proteins. They chose to focus on this pathway to modulate F3 production, largely due to the currently approved use of GSK3 inhibitors for neurodegenerative diseases.
In further analysis of several known GSK3 inhibitors, the compound CHIR99021 (CHIR) was shown to reduce HiBiT F3 secretion up to 76%, and intracellular HiBiT F3 up to 87%. In additional HiBiT F3 cell lines, they showed that treatment with CHIR had no effect on retinal pigment epithelium cell morphology or tight junction formation, and that it reduced the pathology of the most common F3 mutation in vitro. To cap it off, they showed that CHIR reduced the formation of the subretinal basal laminar deposits (BLamDs) that are the central pathologic feature of Ml/DHRD in mice.
Results
The researchers believe this paper represents the first small molecule-based treatment that could be used to treat AMD-like pathology associated with ML/DHRD. In vivo, CHIR not only reduced retinal deposits but did so without causing adverse effects on retinal structure or function. Together, these results suggest that the main pathogenic feature of ML/DHRD (and, more broadly, AMD) could be manipulated using a single small molecule. The authors recommend that more exploration is needed into therapeutic strategies targeting the GSK3 pathway.
Academic Access to New Technologies
The HiBiT cell lines were made possible through the authors’ participation in the Promega Academic Access Program. Non-profit researchers can get affordable early access to the newest Promega technologies through collaboration with Promega R&D. The program is intended to support a partnership between Promega scientists and academic researchers. Products like CRISPR-engineered cell lines, bioassays and cell propagation models help these researchers make significant advances in drug discovery, immune-oncology and many other important areas. By equipping these researchers with cutting-edge tools, the Academic Access Program accelerates scientific discovery, ultimately producing results for real-world problems.
Learn more about the Promega Academic Access Program here.
Read the paper here.
Latest posts by Jordan Villanueva (see all)
- Academic Access to Cutting-Edge Tools Fuels Macular Degeneration Discovery - December 3, 2024
- Novel Promega Enzyme Tackles Biggest Challenge in DNA Forensics - November 7, 2024
- Promega Summer Interns Contribute Skills and Ideas from Logistics to R&D - September 10, 2024
