There is still a lot we don’t know about COVID-19 and the virus, SARS-CoV-2, that caused the pandemic and changed the way we live. But there are two things we do know about the disease: 1) Patients with diabetes and high blood glucose levels are more likely to develop severe COVID-19 symptoms with higher mortality. 2) Patients that experience an uncontrolled inflammatory response, called the cytokine storm, also develop more severe COVID-19 symptoms. The fact that both high glucose levels and an exaggerated immune response drive severe disease suggests that the two may be linked. But how? The answer may lie in the metabolism of immune cells in the lungs of COVID-19 patients, according to a recent study published in Cell Metabolism.
When SARS-CoV-2 enters the host lung cells, it begins to replicate, triggering an immune response that results in a rush of monocytes and macrophages to the infection site. The researchers found that high glucose levels can increase the replication of SARS-CoV-2 within monocytes and cause them to produce more proinflammatory cytokines, such as TNFα, IL-1β and IL-6. High levels of these cytokines are known to contribute to the cytokine storm. Next, the researchers dug deeper to understand how SARS-CoV-2 infection increases cytokine production.
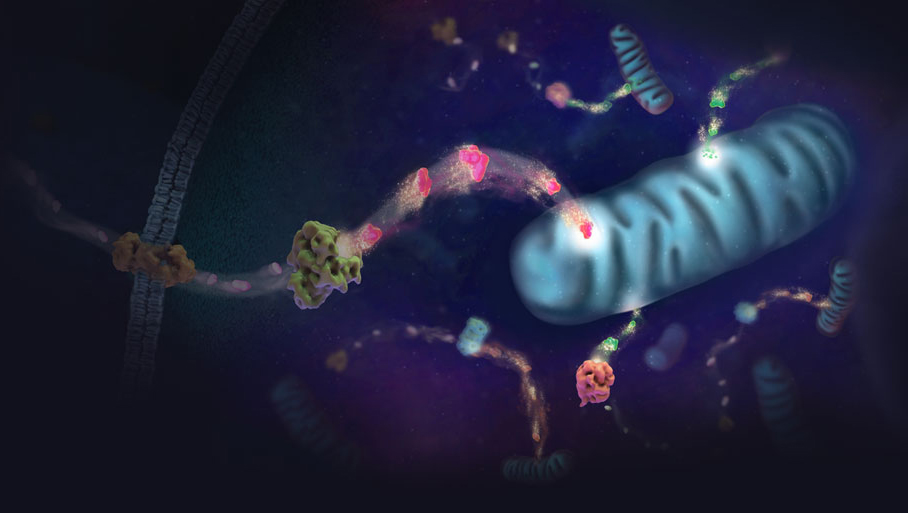
The researchers found that when monocytes are infected with the SARS-CoV-2 virus, their cellular metabolism changes. The monocytes begin using glycolysis as their main source of energy production, instead of oxidative phosphorylation. This change is facilitated by an increase of reactive oxygen species (ROS) generated from the mitochondria. Increased ROS production induces the expression of a key transcription factor called HIF-1α, which controls the expression of other genes involved in glucose transport and glycolysis. As a result, glycolysis increases in infected cells, which then further drives SARS-CoV-2 viral replication and cytokine production in monocytes.
Could this switch in monocyte metabolism directly result in more severe COVID-19 symptoms? Another key predictor of COVID-19 severity is the loss of lymphocytes in the blood, a condition known as lymphopenia. The researchers wanted to know whether the metabolic reprogramming of monocytes under high blood glucose levels could inhibit lymphocyte (T cell) proliferation, potentially causing lymphopenia. Their results showed that SARS-CoV-2 infected monocytes had significantly reduced CD4 and CD8 T cell proliferation. This observation could explain how SARS-CoV-2 infection leads to lymphopenia and severe COVID-19.
The study further showed that, under high glucose conditions, SARS-CoV-2 infection promotes apoptosis in lung epithelial cells, causing increased cell death. Importantly, cell death was prevented when treated with a HIF-1α inhibitor, suggesting that apoptosis is dependent on the activation of HIF-1α and subsequent changes in the glycolysis pathway. This is good news for drug development, as this means there is hope that a drug targeting HIF-1α might be used to treat COVID-19.
In summary, this study showed that a switch in immune cell metabolism could explain how high glucose levels contributes to the cytokine storm and result in severe COVID-19 symptoms. Future studies may explore the use of drugs targeting HIF-1α or other key factors involved in glycolysis to treat COVID-19.
Learn more about interrogating energy metabolism pathways for drug discovery!
Featured Product
The GoScript™ Reverse Transcriptase cDNA synthesis kit was used in this study to reverse-transcribe extracted SARS-CoV-2 RNA.
Related Posts
Latest posts by Johanna Lee (see all)
- Microfluidic Organoids Could Revolutionize Breast Cancer Treatment - March 25, 2025
- Bacteria From Insect Guts Could Help Degrade Plastic - January 28, 2025
- A Diabetes Drug, Metformin, Slows Aging in Male Monkeys - December 19, 2024
