Developing a vaccine that is safe, effective, easily manufactured and distributed is a daunting task. Yet, that is exactly what is needed in response to the COVID-19 pandemic.
Vaccine development, safety and efficacy testing take time. The mumps vaccine is thought to be the quickest infectious disease vaccine ever produced, and its development required four years from sample collection to licensing (2). However, there are many reasons to anticipate quicker development for a COVID-19 vaccine: Researchers are collaborating in unprecedented ways, and most COVID-19 scientific publications are free for all to access and often available as preprints. As of August 11, 2020, researchers around the globe have more than 165 vaccine candidates in development, 30 of which are in some phase of human clinical trials (1). The range of vaccine formulations available to scientists has expanded to include RNA and DNA vaccines, replication-defective adenovirus vaccines, inactivated or killed vaccines and subunit protein vaccines. Equally important is that vaccine developers and researchers have greater access to powerful molecular biology tools like bioluminescent reporters that enable quicker testing and development.
Vaccine Target: SARS-CoV-2 Spike Protein
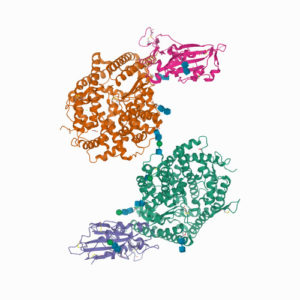
Most vaccines currently in development against SARS-CoV-2 have focused on the SARS-CoV-2 spike (S) protein. This is the protein that protrudes from the virus’ envelope and allows it to bind to the angiotension-converting-enzyme 2 (ACE2) receptor on the surfaces of target cells. This interaction between the virus S protein and the ACE2 receptor triggers the fusion of the virus with the cell membrane of the host cell (3). Scientists have isolated neutralizing antibodies from human serum that bind to the receptor binding domain (RBD) of the SARS spike protein, suggesting that the spike protein is a viable target for producing an effective immune response (4).
An important part of vaccine development is ensuring that the vaccine is not only effective in eliciting an immune response, but that it is also safe. A vaccine should generate an immune response that neutralizes the ability of the virus to infect and cause disease but not a response that itself causes damage to the host. To determine the efficacy and safety of a vaccine-generated immune response, researchers turn to model organisms. Since COVID-19 is a respiratory disease, researchers and vaccine developers want to ensure that a vaccine neutralizes the virus replication without damaging delicate airways and tissues where the virus might be found.
Pseudovirus Neutralization Assays
Pseudotyped viral particles or pseudoviruses enable researchers to characterize the immune response elicited by a vaccine. Pseudotyped viral particles contain the envelope proteins of a known “parent virus” in which the parent binding protein is exchanged for the binding protein of the virus of interest (in this case the S protein of SARS-CoV-2). The pseudotyped virus particle also typically carries a reporter gene, often a gene encoding luciferase or fluorescent protein. The activity of the pseudovirus is monitored by the reporter, which is only expressed and detected if the pseudovirus successfully infects the host cell. If a vaccinated model organism is producing effective neutralizing antibodies, the pseudovirus will be unable to infect the host cell, which can be easily determined by measuring reporter activity. Luciferase-containing pseudoviruses have been used to study several coronaviruses including MERS, SARS-CoV and SARS-CoV-2 (5).
Pseudotyped viruses carrying luciferase reporters have been used to investigate virus neutralization as a result of vaccination with SARS-CoV-2 vaccines currently in development (6,7). In the first study, antibody response after vaccination with the mRNA-1273 vaccine (Moderna) were evaluated. Both ELISA and SARS-CoV-2 pseudovirus neutralization were used to assess response after a first and second vaccination (6). The SARS-CoV-2 pseudovirus was constructed from a lentivirus parent expressing SARS-CoV-2 S protein and a firefly luciferase reporter (6,8,9). The researchers were able to demonstrate S-specific antibody and neutralization activity from the mRNA-1273 vaccine that was higher than reported values for other vaccine types.
The second study (7) similarly used both pseudotyped virus particles to evaluate the immune response resulting from an adenovirus serotype 26 (Ad26) vector-based vaccines that encoded variants of the SARS-CoV-2 S protein.
Visit our website for resources to support:
SARS-CoV-2 Viral Research
SARS-CoV-2 Serology Testing
Live Virus Neutralization Assays
In addition to pseudovirus neutralization assays, both studies also used live virus neutralization assays. A full-length SARS-CoV-2 virus based on the Seattle Washington isolate was designed to express NanoLuc® luciferase and GFP (6,7,10,11). In both cases, these live virus neutralization assays further confirmed that vaccination with the mRNA-1273 vaccine induced S-specific antibody responses that could neutralize virus activity.
Using these reporter viruses the researchers were able to show that vaccination with the two candidate vaccines achieved dose-dependent viral neutralization in animal models, an essential quality for any effective vaccine.
Literature Cited
- Corum, J. et al. (2020) Coronavirus Vaccine Tracker. The New York Times [Internet: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html Accessed August 11, 2020]
- Akpan, N. (2020) Why a Coronavirus Vaccine Could Take Way Longer than A Year. National Geographic: Coronavirus Coverage [Internet: https://www.nationalgeographic.com/science/2020/04/why-coronavirus-vaccine-could-take-way-longer-than-a-year/ Accessed August 11, 2020]
- Lee, J. (2020) How the coronavirus enters host cells and how to block it. Promega Connections. [Internet: https://www.promegaconnections.com/how-the-coronavirus-enters-host-cells-and-how-to-block-it/ Accessed August 11, 2020]
- Kenefick, K. (2020) Neutralizing Antibodies to SARS-CoV-2 Shown to Lessen Infection in Mice. Promega Connections [Internet: https://www.promegaconnections.com/neutralizing-antibodies-to-sars-cov-2-shown-to-lessen-infection-in-mice/ Accessed August 11, 2020]
- Hooper, K. (2020) Choices for Measuring Luciferase-Tagged Reporter Pseudotyped Viral Particles in Coronavirus Research. [Internet: https://www.promegaconnections.com/choices-for-measuring-luciferase-tagged-reporter-pseudotyped-viral-particles-in-coronavirus-research/ Accessed August 11, 2020]
- Corbett, K.S. et al. (2020) Evaluation of the mRNA-1273 Vaccine against SARS-CoV-2 in Nonhuman Primates. New Eng. J. Med. DOI: 10.1056/NEJMoa2024671
- Mercado, N.B. et al. (2020) Single-shot Ad26 Vaccine Protects against SARS-CoV-2 in rhesus macaques. Nature https://www.nature.com/articles/s41586-020-2607-z
- Wang, L. et al. (2015) Evaluation of Candidate Vaccine Approaches for MERS-CoV. Nat. Commun. 6, 7712.
- Jackson, L. et al. (2020) An mRNA Vaccine against SARS-CoV-2—Preliminary Report. New. Eng. J. Med. DOI: 10.1056/NEJMoa2022483
- Hou, Y.J. et al. (2020) SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract. Cell 183, 429–46.
- Scobey, T. et al. (2013) Reverse genetics with a full-length infectious cDNA of the Middle East respiratory syndrome coronavirus. Proc. Nat. Acd. Sci. 110, 16157–62.
Related Posts
Michele Arduengo
Latest posts by Michele Arduengo (see all)
- An Unexpected Role for RNA Methylation in Mitosis Leads to New Understanding of Neurodevelopmental Disorders - March 27, 2025
- Unlocking the Secrets of ADP-Ribosylation with Arg-C Ultra Protease, a Key Enzyme for Studying Ester-Linked Protein Modifications - November 13, 2024
- Exploring the Respiratory Virus Landscape: Pre-Pandemic Data and Pandemic Preparedness - October 29, 2024

2 comments